Your physician has determined that a colonoscopy is necessary for further evaluation or treatment of your condition. This brochure has been prepared to help you to understand the procedure. It includes answers to questions patients ask most frequently. Please read it carefully. If you have additional questions, please feel free to discuss them with our staff pior to the procedure.
What is a Colonoscopy?
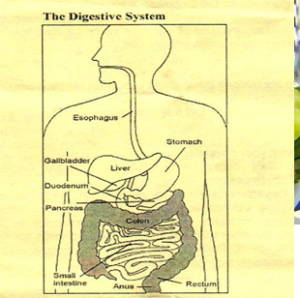
Colonoscopy (koh-luh-NAH-skuh-pee) lets the physician look inside your entire large intestine, from the lowest part the rectum, all the way up through the colon to the lower end of the small intestine. The procedure is used to look for early signs of cancer in the colon and rectum. It is also used to diagnoses the causes of unexplained changes in bowel habits. Colonoscopy enables the physician to see inflamed tissue, abnormal growths, ulcers, bleeding and any abnormalities.
What should you expect?
Colonoscopy is usually well tolerated any rarely causes much pain. There is often a feeling of pressure, bloating or cramping at times during the procedure. For the procedures, you will be given pain medication and a mild sedative to keep you comfort,able and to help you relax during the exam. The physician will insert a long, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a colonoscopy (koh-LoN-oh-skope). The scope transmits an image of the inside of the colon, so the physician can carefully examine the lining of the colon. The scope bends, so the physician can move it around the curves of your colon. You may be asked to change position occasionally to help the physician move the scope. The scope also blows air into your colon, which inflated the colon and helps the physician see better. The colonoscopy takes 15 to 60 minutes.
What if the Colonoscopy shows something abnormal?
If a colonoscopy is being performed to identify sites of bleeding, the areas of bleeding may be controlled through the colonoscopy by injecting certain medications or by coagulation.
If anything abnormal is seen in your colon, like a polyp or inflamed tissue, the physician can remove all or part of it using tiny instruments passed through the scope. That tissue (biopsy) is then sent to a lab for testing.
If there is bleeding in the colon, the physician can pass a heater probe, or electrical probe, or inject special medicines through the scope and use it to stop the bleeding. Remember, that the biopsies are taken for many reasons and do not mean that cancer is suspected.
What are polyps, how and why they are removed?
Polyps are abnormal growths from the lining of the colon which vary in size from a tiny dot to several inches. The majority of polyps are benign (non-cancerous) but he doctor cannot always tell a benign from a malignant (cancerous) polyp by its outer appearance alone. For this reason, removed polyps are sent for tissue analysis. Removal of colon polyps is an important means of preventing colorectal cancer. Tiny polyps may be totally destroyed by fulguration (burning), but larger polyps are removed by a technique called snare polypectomy. The doctor passes a wite loop (snare) through the colonoscopy and severs the attachment of the polyp from the intestinal wall by means of electrical current. You should feel no pain during the polypectomy. Although even gastroenterologists may refer a patient with a large polyp to a special expert in the removal of polyps, a trained colonoscopist can remove the overwhelming majority of routine polyps.
What happens after a Colonoscopy, how will K feel?
Your physician will explain the results to you and advise you when to follow-up. You will be given discharge orders when you areready to leave. If you have any questions, please call our office.
You may have some cramping or bloating because of the air introduced tint the colon during the examination. This should disappear quickly with the passage of flatus (gas).
Generally, you should be able to eat after leaving endoscopy, but your doctor may restrict your diet and activities especially after polypectomy.
Preparation
Your colon must be completely empty for the colonoscopy to be thorough and safe. You will be given detailed instructions when you are scheduling your procedure. To prepare for the procedure you will follow a liquid diet as described in the instructions you will receive from our office. You will also take one of several types of laxatives the night before the procedure. Also you must arrange for someone to take you hame afterward—you will not be allowed to drive due to the sedatives. Inform your physician of any medical conditions or medications that you are currently taking, prior to the colonoscopy. You may brush your teeth, but do not swallow the water.
The day of the procedure you will arrive at the time specified, which is one hour prior to the procedure scheduled start time.
Medications
Most medicines may be continued as usual, but some medications can interfere with the preparation of/or the procedure itself. It is therefore best to inform your physician of your current medications, anticoagulants (blood thinners). Insulin and iron products are examples of medications whose use should be discussed with your physician prior to the procedure.
You should alert your doctor if you require antibiotics prior to undergoing dental procedures, since you may need antibiotics prior to the colonoscopy as well.
Routine medications can be taken the morning of the procedure with a very small sip of water. This does not include taking any of the medications listed above.
What are the possible complications?
Bleeding and puncture of the colon are possible complications of colonoscopy. However, such complications are uncommon. Bleeding may occur from the site of biopsy or polypectomy. It is usually minor and stops on its own or can be controlled through the colonoscope. There is a small risk that removing a polyp will cause bleeding or result in a burn to the wall of the colon, which could require emergency surgery. Other potential risks include a reaction to the sedatives used and complications from heart or lung disease. Localized irritation of the vein where medications were injected may rarely cause a tender lump lasting for several weeks, but this will go away eventually. Applying hot packs or hot moist towels may help relieve discomfort.
Cost of the procedure, methods of billing, insurance coverage
A staff member will be contacting you from the facility where the colonoscopy is scheduled, to pre-register you for the procedure. You should receive this call no later than 2 days prior to the procedure. Please contact our office immediately if you do not receive this call.
You will be billed separately for the physician’s services as well as the facilities charges.
Most insurances cover this procedure, however to be prepared, you may want to contact your insurance company to be sure that the procedure is covered. All applicable deductibles and xo-pays will apply.
Our office will coordinate with the facility the scheduling of your procedure: you do not need to schedule the procedure with the facility yourself.
We will also obtain the necessary, the day of the procedure at the facility. Our office will bill you for any co-pay/deductible after we receive payment from your insurance company.
What is Colorectal Cancer?
Colorectal cancer is the second most common cancer killer in the United States, causing an estimated 55,000 deaths each year. More than 138,000 new cases of colorectal cancer are diagnosed each year. Men and women are equally affected by this disease. Colorectal cancer is cancer of the colon and rectum, two parts of the digestive system also known as the large intestine. Most colon cancers arise from polyps are identified at a very early stage, they can be removed before they become cancerous. Complications of colorectal cancer can be reduced or even prevented with the simple step of regular screening.
Who is at risk for Colorectal Cancer?
Women are just as likely as men to develop colorectal cancer. Colon cancer is most common after age 50, but the chances of developing this disease increase after age 40. Close relatives of a person who has had colorectal cancer before the age of 55, or persons with one of several chronic digestive conditions have a higher than average risk of developing colorectal cancer.
What are the symptoms of colorectal Cancer?
Most early cancers produce no symptoms, which is why screening is so important. Some possible symptoms, listed below, certainly do not always indicate the presence of colorectal cancer, but should prompt a visit with your physician for a check-up.
- Frequent gas pains
- Blood in or on the stool
- Diarrhea or Constipation
- A feeling that the bowel has not emptied completely
Regular screening is the absolute best protection against Colorectal Cancer. When should you be screened for colorectal Cancer?
The screening program recommended by the American College of Gastroenterology (ACG) includes:
RISK CATEGORY INCREADED Average
DEFINITION
- Age 50 or older and no other risk factors
AGE TO START CSREENING
- 50 YEARS
ACG RECOMMENDED SCREENING
- Colonoscopy every 10 years
RISK CATEGORY Moderately
Increase
DEFINITION
- One first degree relative (immediate family member-mother, father, brother, sister) with colorectal cancer diagnosed at age 60 or older
ACG RECOMMENDED SCREENING
- Colonoscopy at least every 10 years
RISK CATEGORY High
DEFINITION
- Two or more first degree relatives (immediate family member-mother, father, brother, sister) with colorectal cancer or one diagnosed with colorectal cancer at age less than 60
AGE TO STAR SCREENING
- 40 years or 10 years younger than age at diagnosis of the youngest affected relative, whichever is earlier
ACG RECOMMENDED SCREENING
- Colonoscopy every 3 to 5 years
To the patient
Because education is an important part of comprehensive medical care, you have been provided this information to prepare you for this procedure. If you have questions about your need for colonoscopy, alternative tests, the cost of the procedure, methods of billing or insurance coverage, do not hesitate to speak with our staff.
Thank you …….
We are pleased that you and your physician have selected our office to fulfill your medical needs. If ever have any questions, please feel free to contact our staff at 301-856-1960
